Why should I learn about bats and rabies?
Most of the recent human rabies cases in the United States have been caused by rabies virus from bats. Awareness of the facts about bats and rabies can help people protect themselves, their families, and their pets. This information may also help clear up misunderstandings about bats.
When people think about bats, they often imagine things that are not true. Bats are not blind. They are neither rodents nor birds. They will not suck your blood -- and most do not have rabies. Bats play key roles in ecosystems around the globe, from rain forests to deserts, especially by eating insects, including agricultural pests. The best protection we can offer these unique mammals is to learn more about their habits and recognize the value of living safely with them.
How can I tell if a bat has rabies?
Rabies can be confirmed only in a laboratory. However, any bat that is active by day, is found in a place where bats are not usually seen (for example, in a room in your home or on the lawn), or is unable to fly, is far more likely than others to be rabid. Such bats are often the most easily approached. Therefore, it is best never to handle any bat.
What should I do if I come in contact with a bat?
If you are bitten by a bat -- or if infectious material (such as saliva) from a bat gets into your eyes, nose, mouth, or a wound -- wash the affected area thoroughly and get medical advice immediately. Whenever possible, the bat should be captured and sent to a laboratory for rabies testing (see: How can I safely capture a bat in my home?).
People usually know when they have been bitten by a bat. However, because bats have small teeth which may leave marks that are not easily seen, there are situations in which you should seek medical advice even in the absence of an obvious bite wound. For example, if you awaken and find a bat in your room, see a bat in the room of an unattended child, a sleeping, mentally impaired or intoxicated person, try to safely contain the bat using the safety precautions listed below. This is a potential exposure and should be reported. To report a bat exposure use the bite form or call our office during business hours. If the bat has died, use gloves to put it in a secure container and keep it cool but not frozen so it can be tested for Rabies. Seek medical advice.
People cannot get rabies just from seeing a bat in an attic, in a cave, or at a distance. In addition, people cannot get rabies from having contact with bat guano (feces), blood, or urine, or from touching a bat on its fur (even though bats should never be handled!).
What should I do if my pet is exposed to a bat?
If you think your pet or domestic animal has been bitten by a bat, contact a veterinarian or the Environmental Health Division for assistance immediately and have the bat tested for rabies. Remember to keep vaccinations current for cats, dogs, and other animals.
How can I keep bats out of my home?
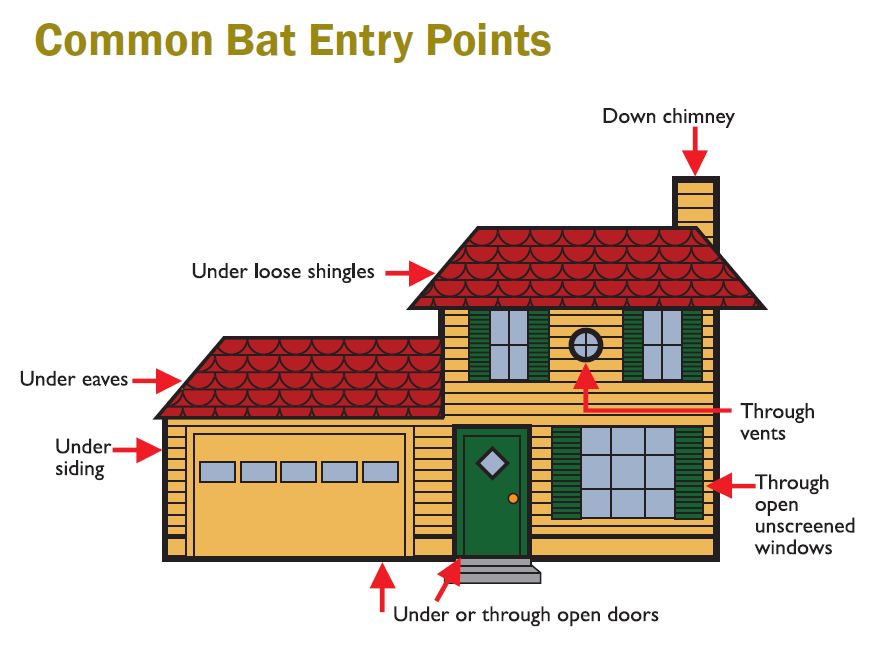
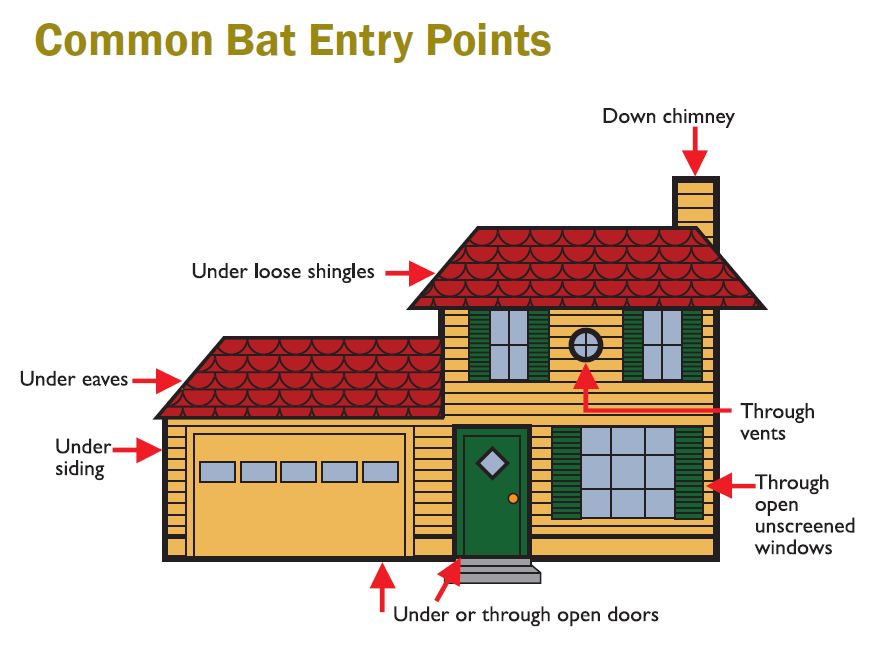
Some bats live in buildings, and there may be no reason to evict them if there is little chance for contact with people. However, bats should always be prevented from entering rooms of your home. For assistance with "bat-proofing" your home, contact an animal-control or wildlife conservation agency. If you choose to do the "bat-proofing" yourself, here are some suggestions. Carefully examine your home for holes that might allow bats entry into your living quarters. Any openings larger than a quarter-inch by a half-inch should be caulked. Use window screens, chimney caps, and draft-guards beneath doors to attics, fill electrical and plumbing holes with stainless steel wool or caulking, and ensure that all doors to the outside close tightly.
Additional "bat-proofing" can prevent bats from roosting in attics or buildings by covering outside entry points. Observe where the bats exit at dusk and exclude them by loosely hanging clear plastic sheeting or bird netting over these areas. Bats can crawl out and leave, but cannot re-enter. After the bats have been excluded, the openings can be permanently sealed. For more information about "bat-proofing" your home, contact Bat Conservation International.
Things to remember when "bat-proofing"
During summer, many young bats are unable to fly. If you exclude adult bats during this time, the young may be trapped inside and die or make their way into living quarters. Thus, if possible, avoid exclusion from May through August.
Most bats leave in the fall or winter to hibernate, so these are the best times to "bat-proof" your home.
How can I safely capture a bat in my home?
If a bat is present in your home and you cannot rule out the possibility of exposure, leave the bat alone and contact an animal-control or Environmental Health Division for assistance. If professional help is unavailable, use precautions to capture the bat safely, as described below.
What you will need:
- leather work gloves (put them on)
- small box or coffee can
- piece of cardboard
- tape
When the bat lands, approach it slowly, while wearing the gloves, and place the box or coffee can over it. Slide the cardboard under the container to trap the bat inside. Tape the cardboard to the container securely, and punch small holes in the cardboard, allowing the bat to breathe. Contact the Environmental Health Division or animal-control authority to make arrangements for rabies testing.
If you see a bat in your home and you are sure no human or pet exposure has occurred, confine the bat to a room by closing all doors and windows leading out of the room except those to the outside. The bat will probably leave soon. If not, it can be caught, as described, and released outdoors away from people and pets.
Are bats beneficial?
Yes. Worldwide, bats are a major predator of night-flying insects, including pests that cost farmers billions of dollars annually. Throughout the tropics, seed dispersal and pollination activities by bats are vital to rain forest survival. In addition, studies of bats have contributed to medical advances including the development of navigational aids for the blind. Unfortunately, many local populations of bats have been destroyed and many species are now endangered.
Where can I learn more about bats?
Contact your state or local wildlife conservation agency or:
Bat Conservation International, Inc.
www.batcon.org
To learn more about endangered bats and the Endangered Species Act, Contact the US Fish and Wildlife Service:
U.S. Fish and Wildlife Service
Division of Endangered Species
www.fws.gov
Where can I learn more about rabies?
Contact the Waukesha County Environmental Health Division
or:
Centers for Disease Control and Prevention
National Center for Infectious Diseases
www.cdc.gov/ncidod/dvrd/rabies